- Christina Sumners
- COVID-19, Healthy Living, Medicine, Show on VR homepage
Glossary of terms for the COVID-19 age
What's the difference between social distancing, quarantine and self-isolation? What's flattening the curve? A physician breaks down terms commonly associated with COVID-19
Brandon Williamson, MD, a physician Texas A&M Health Family Care and a clinical assistant professor at Texas A&M College of Medicine, helps us present some terms that the novel coronavirus pandemic has brought into our vocabularies.
Coronavirus and COVID-19
Coronaviruses have been around for a long time. They’re a large family of viruses that affect both humans and animals. In humans, coronaviruses are responsible for some cases of the common cold as well as more serious illnesses, like pneumonia. Their first part of the name, “corona,” comes from the crown-like spikes on their surfaces. Scientists have discovered hundreds of coronaviruses to date.
The most recent coronavirus is related to two others that have made news in recent years: severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS).
The newly discovered coronavirus causes an infectious disease called COVID-19 (short for “coronavirus disease 2019”). It emerged in the Wuhan province of China in December 2019 before circulating worldwide.
Most people who have COVID-19 experience cold-like symptoms, such as fever, body aches, fatigue and cough. In severe cases, patients experience shortness of breath that sometimes requires hospitalization and even a breathing machine, called a ventilator.
Outbreak, epidemic and pandemic
An outbreak is when a disease occurs in a particular location at a higher rate than normal. Some outbreaks are expected, such as yearly outbreaks of the flu. COVID-19 began as an outbreak in Wuhan, China in November 2019. The terms epidemic and pandemic describe the size and spread of an outbreak.
An epidemic is when a disease spreads rapidly, usually affecting a large number of people. Basically, an outbreak becomes an epidemic when it spreads rapidly beyond a particular location or community to others nearby.
A pandemic is a step above an epidemic. It denotes the rapid spread of a disease throughout several countries and continents and affects a large population. The World Health Organization (WHO) declared COVID-19 a pandemic on March 11, 2020.
Community spread, community transmission and contact tracing
Community spread and community transmission are used interchangeably. Community spread relates to how people become infected with a virus in a given area. Early cases of COVID-19 could be traced to travel to and from areas experiencing an outbreak of the virus, or direct contact with people who had traveled in those areas. As the pandemic grew, patients who had not traveled, or been in direct contact with someone who had, started testing positive. That meant the virus had shifted to community spread. Community spread is a concern because it is almost impossible to trace where the patient was infected in the first place or who else the patient may have infected afterward.
The process of figuring out where, when and how a patient was infected and who that patient may have infected afterward is called contact tracing. Contact tracing is an important part of understanding how an infectious disease spreads and keeping the disease contained. If health care providers can trace the spread of the virus for individual patients, they can identify others who may need testing or medical care, or who need to self-quarantine in order to keep the virus from spreading to others.
Currently the only way to engage in contact tracing is through interviews with infected people. This process is lengthy and difficult because nobody can remember every single person they have been in close proximity to on any given day. However, Apple and Google announced that they are going to collaborate on software to help with contact tracing. The idea is that Android phones and iPhones equipped with the latest updates would help to record who has been in contact with whom.
Social distancing, quarantine and self-isolation
People worldwide have had to practice social distancing in order to slow the spread of COVID-19. Social distancing refers to several measures that promote physical distance among people. Measures include maintaining at least 6 feet between yourself and others when in public places, working and attending school from home, only leaving home for essential needs and activities, and avoiding contact with anyone outside the household. Recently media sources have been using the term physical distancing in place of social distancing, in order to clarify that although people need to stay physically apart, they should continue to stay socially connected with friends and family through a variety of distance activities and communication.
Social distancing is a preventive measure that everyone practices, but quarantine applies strictly to individuals who have been exposed to the virus but are not showing any symptoms. The intent of quarantine is to keep people who have been exposed to the virus away from people who have not been exposed. During quarantine, the exposed individual should avoid public places and physical contact with others. The length of time someone needs to be quarantined relates to the incubation period of the virus, which is at most 14 days for COVID-19.
The most extreme measure is self-isolation, which applies to anyone who contracts COVID-19 and experiences symptoms. Self-isolation takes quarantine a step further by keeping the ill person separate from everyone else, even other people who live in the same house. It involves having a room designated for the person in isolation, a separate bathroom from the rest of the residents (if possible) and contact with only one individual designated as a caregiver if one is needed.
Reproductive Rate (R0)
The reproductive rate (R0) is used to describe the contagiousness of a disease. It is estimated with a complex mathematical model, but the number it generates tells us roughly how many people one person will infect if they have the virus and don’t take any measures against infecting others.
Any reproductive rate below 1 tells us that it is unlikely the virus will be transmitted, but anything above one means at least one person will be infected. The reproductive rate for seasonal influenza is around 1.2 to 1.3, which means that if you were infected with influenza, you are highly likely to pass it onto at least one other person.
The reproductive rate for COVID-19 is still being determined, but several sources indicate it averages around 2.5. That means that on average, two to three people will be infected for each individual who has the virus and doesn’t take any measures to keep from passing it on to others.
If one person is infected, it is likely they will infect one other person they come into contact with. Then, that one person will infect one other person, and the result is a chain totaling three infections. On the other hand, a person with COVID-19 is likely to infect two other people. Then, each of those people are likely to infect two more people. This leads to seven infections overall. Staying at home and practicing social distancing can alleviate this level of spread.
Incubation period
The incubation period of a disease is the time from which a person is first exposed until they develop the first symptoms. Evidence shows that the incubation period for COVID-19 ranges from two to 14 days. What is important to know is that a person might be contagious throughout the incubation period, regardless of whether the person has symptoms.
PPE, surgical mask, respirator and ventilator
PPE is short for personal protective equipment and refers to special clothing or gear used to prevent contact with infectious or hazardous materials. Currently, the PPE worn by health care workers to protect them from COVID-19 includes gloves, gowns, shoe/boot covers, surgical masks, respirators, face shields and goggles or safety glasses.
Surgical masks, or face masks, are loose-fitting masks that cover the nose and mouth. They are designed to protect the wearer from large particles, splashes, droplets or sprays that may contain germs, and may protect others from the wearer’s saliva and other bodily fluids. The masks are made from different materials, and their design determines their level of protection and how easy it is to breathe while wearing the mask. They will not protect the wearer from all germs and contaminants because they are not designed to filter small particles and they do not seal around the mouth and nose.
On the other hand, respirators are masks that are specially fitted to create a seal around the nose and mouth, and they keep out at least 95 percent of airborne germs and contaminants. They are also called N95 masks. The N95 masks worn by health care workers are in short supply.
Finally, a ventilator is a very different piece of equipment. Ventilators are not a type of PPE; they are machines that deliver air to a patient’s lungs when the patient cannot breathe properly. Hospitals keep a limited number of ventilators on hand. Patients hospitalized with COVID-19 tend to experience breathing problems and need access to ventilators; therefore, many hospitals could face shortages of the equipment.
Stay-at-home order, shelter-in-place order and lockdown
For the purposes of the COVID-19 pandemic, the three terms stay-at-home order, shelter-in-place order and lockdown are often used interchangeably. All three of these terms mean that residents must remain at home, except when it is absolutely necessary. Stay-at-home and shelter-in-place orders are legal terms, so there could be fines or imprisonment for violators.
Traditionally, shelter-in-place applies to natural disasters and other events and indicates that people should remain where they are until the danger is over. A lockdown, on the other hand, is used in events such as mass shootings, but is also intended to keep people safe.
Essential and nonessential activities and services
These terms are related to stay-at-home orders. Staying at home is a relatively easy way to keep people physically separate from others. However, people still need essential services, such as groceries, medications and emergency medical care. The leaders in each county, state or country determine what is essential versus nonessential based on location and culture. Generally speaking, essential services include grocery stores, pharmacies, gas stations and banks; however, check your local area to see if there are other businesses and services considered to be essential.
In addition to essential services, there are also essential activities, which are things people need to do in order to live. For example, there are still people who need to go to work in order for others to have access to health care and necessities, so going to work would be an essential activity for these individuals. While engaging in essential activities, it is important to continue to practice social distancing whenever possible and to wear a mask.
Nonessential activities and services refer to anything that is not considered necessary for daily living, such as entertainment, sit-in dining, grooming and leisure.
Telehealth and telemedicine
Telehealth refers to a collection of technologies and services that improve patient care and the health care delivery system overall. Telehealth includes remote clinical services, provider training, administrative meetings and continuing medical education, as well as clinical services. It allows health care providers and employees to work together and learn. It also allows patients access to health care providers and services, regardless of their physical location.
Another term closely related to telehealth is telemedicine. Telemedicine relies on technology, such as videoconferencing and remote patient monitoring, to provide real-time health care to patients, regardless of their location. Telemedicine is different from telehealth because it specifically applies to patients and health care providers, while telehealth includes the entire health care system. Telemedicine has become increasingly more popular since the pandemic has limited in-person office visits for patients and their providers.
Flattening the curve
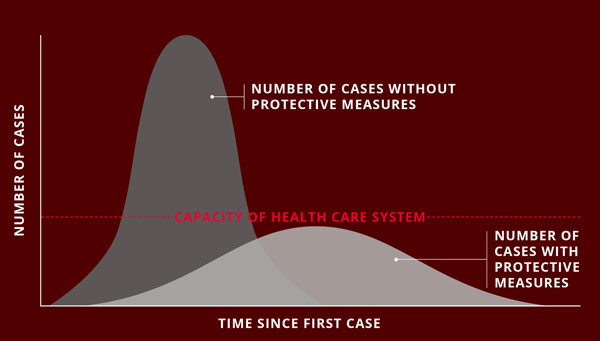
The idea of flattening the curve refers to a graph with two curves. Each curve represents how many people are infected by COVID-19 over time, beginning with the first case. There is a taller curve, which peaks closer in time to the first case, and a shorter, flatter curve that peaks further away from the first case. The taller curve is what happens if the virus is left to spread freely through the population. In this case, the higher, faster peak of cases makes it difficult for hospitals to keep up with treatment. Using preventative measures like social distancing and staying at home is how we get the shorter curve. If we slow the spread of the virus, it may take longer to get to a peak number of cases, but it makes it easier for hospitals to keep up with patients’ care.
Testing
There are two types of tests related to COVID-19. One type of test determines whether a person has the COVID-19 virus. This test generally has been restricted to people who have symptoms because early in the pandemic the number of test kits available was very limited. However, testing capabilities are slowly expanding.
The second type of test determines if there are COVID-19 antibodies present in a person’s blood. Antibodies are small proteins that fight off diseases. So, this test can show if a person has ever had the virus, even if they have never had any symptoms.
Symptomatic and asymptomatic
When a person is symptomatic, it means that they have contracted COVID-19 and are displaying symptoms of the virus. When a person is asymptomatic it means that they are not showing signs of COVID-19 infection. It is important to remember that a person can be exposed to COVID-19 and pass the virus on to others even though they are asymptomatic.
Immunocompromised, high-risk
People who are immunocompromised have weakened immune systems. Usually these people know who they are, but the group generally includes cancer patients, people with autoimmune conditions and pregnant women. Because of their weakened immune systems, they are more vulnerable to contracting COVID-19, and if they do, their symptoms are likely to be more severe than someone with a healthy immune system.
The term high-risk includes those who are immunocompromised but goes further to include individuals over 65, people living in nursing homes and long-term care facilities, and people who have chronic illnesses or underlying health conditions. Some people with chronic illnesses, such as those with asthma, may be at higher risk of becoming severely ill if they do contract the virus, but are not necessarily at higher risk of becoming infected.
Morbidity rate and mortality rate
Although these two terms sound similar, their meanings are quite different. The morbidity rate refers to the number of people who have contracted an illness relative to the overall population. The mortality rate refers to how many people have died from an illness relative to the overall population.
~Written by September Martin
Media contact: media@tamu.edu


