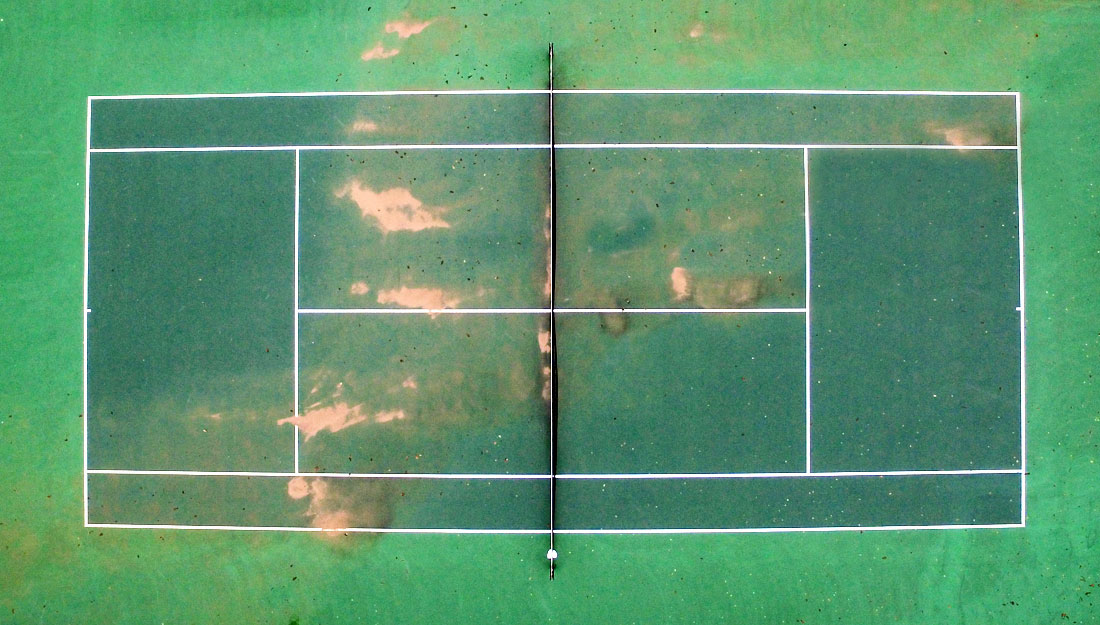
Protecting an area the size of a tennis court: The lining of your gut
Any number of things can cause inflammation, and sometimes this is a protective response, like when the body musters its resources to heal an injury or fight off an invading infection. However, over the long term, inflammation of the gut lining is damaging and can lead to diseases from diabetes and metabolic syndrome to inflammatory bowel disease (IBD) like ulcerative colitis and Crohn’s disease, and even to different cancers.
The research team of Narendra Kumar, Ph.D., associate professor of pharmaceutical sciences, and Jayshree Mishra, Ph.D., research assistant professor, both at the Texas A&M Irma Lerma Rangel College of Pharmacy, have been studying inflammation for years. They want to understand the mechanism, which is the first step to ultimately being able to have a prevention or a cure. “Genetics plays a huge role, but so does environment,” Kumar said. They would like to be able to tease out exactly how each contributes.
“The surface area of the mucosal lining in the gastrointestinal tract is roughly the size of a tennis court,” Kumar said. “It is 100 times larger than the area of the skin, and we’re exposed to the environment far more through our gut than through our skin, yet relatively little attention has been focused on it.” He suggests that new ways need to be developed to protect the gut lining, just like we use sunscreen and other methods to protect skin.
Kumar, Mishra and their team have recently published new research that sheds some light on the mechanism of gut mucosal inflammation and the molecular determinants that regulate it. One of those regulatory elements is an enzyme called Janus kinase 3, or Jak3. As levels of Jak3 go down, the chances of developing metabolic syndrome go up. People born without working Jak3 have severe immune deficiency—so much so that a simple infection can kill them and they die within the first year of life without a bone marrow transplant. Those with a polymorphic form, which means they have some Jak3 but not as much as other people, will be far more likely to have metabolic syndrome.
Although it may seem strange that an enzyme that has such profound effects on the immune system also seems to impact metabolic conditions, the explanation goes back to inflammation.
The mucosal layer in the gut acts as a barrier to outside contaminants and pathogens, just like skin does. In the case of the gut, it also has to distinguish the “good” residential microbiota from foreign invaders. Kumar suggests thinking of the gut as being two types of barriers in one. First is the physical barrier, like a fence, that keeps things out. The second is a functional barrier, which is like a sensor. It determines friend from foe, and when it senses a foe, it signals the immune system to attack. These sensors also detect endotoxins, which are present in the cell walls of microbiota, and a high-fat diet acts very similarly to an endotoxin. Sometimes this system goes awry, and the immune cells attack food or harmless bacteria, which leads to one of about 200 possible autoimmune diseases. For a visual explanation of the process, the journal Nature has created a video.
In healthy people, the barrier is re-established quickly after a breach, and the acute inflammation and immune reaction dies down. If this doesn’t happen, though, chronic low-grade inflammation occurs. One result can be a lack of satiety signals and an inability to detect insulin appropriately, which leads to insulin resistance, and eventually Type 2 diabetes. Chronic inflammation can also lead to IBD, which itself can progress into IBD-associated colorectal cancer.
Eventually, Kumar and Mishra and their team hope to be able to develop some sort of intervention to stop these cascades of negative effects. At the moment, their best advice is to eat healthy foods and consider a daily probiotic, but they also urge caution. “There’s still work to be done in this area,” Mishra said. “We have to find out what kinds of probiotics to use—which ones are beneficial and in what combinations.”
But the first step is determining who has the low-grade chronic inflammation. To this end, they’ve partnered with hospitals in South Texas to begin a study early next year to test their non-invasive way of determining if a patient has low-grade chronic inflammation. “We want to contribute to the health of area residents by helping to understand the onset, progression and establishment of chronic inflammation so we can discover a preventive measure or a therapy to reverse the inflammation.”
The group also plans to determine the prevalence of the Jak3 gene polymorphism in different populations, and if this variation predisposes different groups toward diabetes or any other health complications.
“There’s an age-old saying, ‘Go by your gut,’ and it looks like that is scientifically important,” Kumar said. “It’s all about taking care of the gut mucosa, which you can do through eating well and getting exercise.”
Media contact: media@tamu.edu


