- Christina Sumners
- Medicine, Research, Show on VR homepage
Shedding light on cognitive aging
A neuroscientist combines novel genetic and engineering tools to explore age-related decline in mental skills
Nerve cell
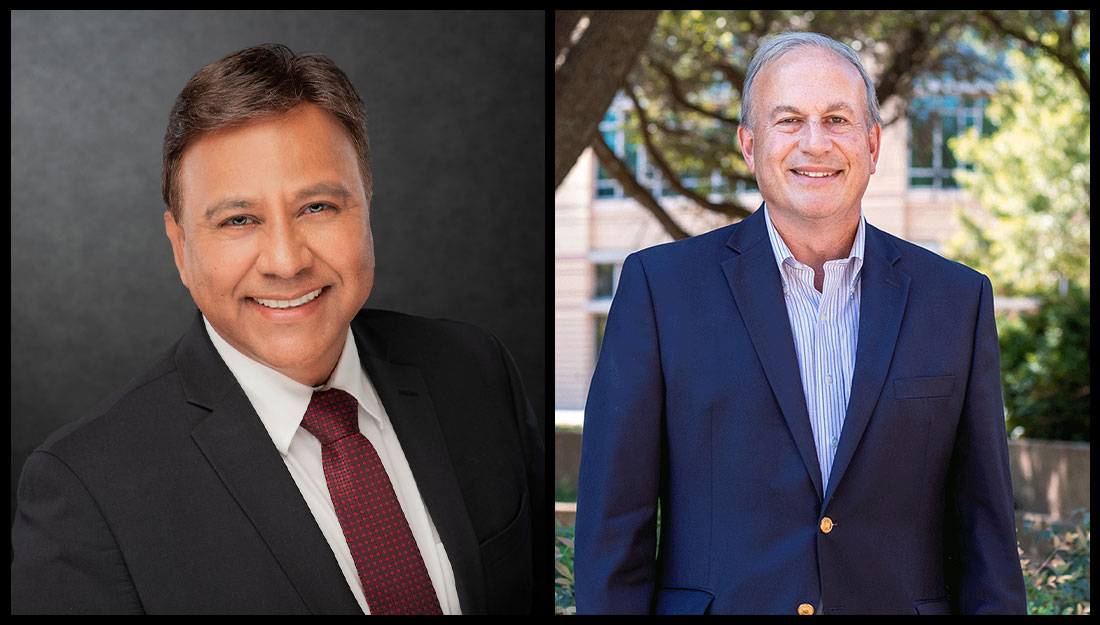
Why does aging cause severe deterioration in memory and thinking abilities in some people and not in others? Neuroscientist William Griffith, PhD, Regents Professor and department head at Texas A&M College of Medicine, is merging tools from neuroscience and engineering to investigate the neural basis of cognitive decline with age.
Griffith and his team look at age-related changes in electrical properties of neurons and their impact on neuronal communication. “We’re interested in studying properties of synaptic transmission and neuronal properties in parts of the brain important in cognitive behavior,” he said.
Much of Griffith’s research focuses on the part of the brain that undergoes neurodegeneration in Alzheimer’s disease. This region, called the basal forebrain (BF), contains a variety of cells. However, BF cholinergic neurons (the cells that use the neurotransmitter acetylcholine for communication) make dense interconnections with other parts of the brain involved in memory and attention. Thus, a loss of BF cholinergic cells, as in Alzheimer’s, contributes to a progressive cognitive decline.
Earlier work from Griffith’s team showed that the delicate balance of calcium ions across cholinergic neurons’ cell membranes is altered in aged animal models showing signs of cognitive decline. These results suggested that calcium ion-dependent functions such as synaptic transmission of cholinergic cells might also be affected. Over time, these changes could cause BF cholinergic cells to function abnormally.
Although investigating the electrical properties of cholinergic synapses was the logical next step, Griffith realized that traditional tools did not suit this purpose. “The basal forebrain is a large network of different kinds of cells,” he said. “We couldn’t specifically stimulate one kind of cell and study its properties because if you electrically stimulate, you non-specifically stimulate everything.”
To overcome this obstacle, Griffith recently turned to optogenetics—a technique by which specific neurons can be genetically engineered to respond to light rather than electrical current. By expressing light-sensitive proteins called opsins in subsets of neurons innervating cholinergic cells, his team can now turn on specific synapses in the BF using light and examine their properties.
Soon, Griffith plans to study age-related cognitive decline in vivo. For this project (which made it to the semifinal round for the X-Grant awards this year), he will use a combination of optogenetics and engineering devices based on feedback information called “closed-loop” systems. Just as insulin pumps inject the correct amount of insulin based on the feedback information on circulating blood glucose levels, a closed-loop system stimulates neurons based on their ongoing activity. In particular, if a neuron is less active than normal, it could be stimulated more.
Griffith is currently collaborating with Sung Il Park, PhD, assistant professor at the Texas A&M College of Engineering, who has designed a wireless closed-loop miniature system for optogenetics.
Park’s closed-loop device—small enough to be implanted on the skull of a small animal model—can be used to track neuronal activity in real time and provide light stimulation on a feedback basis while the animal model is performing a cognitive task. Griffith hopes that by rectifying aberrant activity of BF neurons, age-related cognitive impairments can be corrected.
Griffith notes that optogenetics-based stimulating systems offer another advantage over conventional stimulating techniques such as deep brain stimulation (DBS): “When you do DBS, an electrode placed in a certain part of the brain stimulates non-specifically. But with optogenetics, we can get selective stimulation of a subset of neurons,” he said.
Within the next decade or two, Griffith hopes that technologies such as optogenetics and closed-loop systems will be a part of mainstream medicine to treat a variety of neurological conditions. “Historically, we have had limited success treating neurological diseases. We can treat some of the symptoms of Parkinson’s disease or dementia, but currently, we cannot cure any of these diseases,” he said. “With the advent of new technologies like optogenetics there is the potential for game-changing translational therapeutic approaches—to treat neurological diseases like we have never seen before.”
Article written by Vandana Suresh
Media contact: media@tamu.edu