- Valerie Vierkant
- Medicine, Research, Show on VR homepage
Nasal spray made from stem cell-derived vesicles could treat Alzheimer’s disease
Innovative new research from the College of Medicine offers hope for delaying Alzheimer’s disease progression by years after initial diagnosis
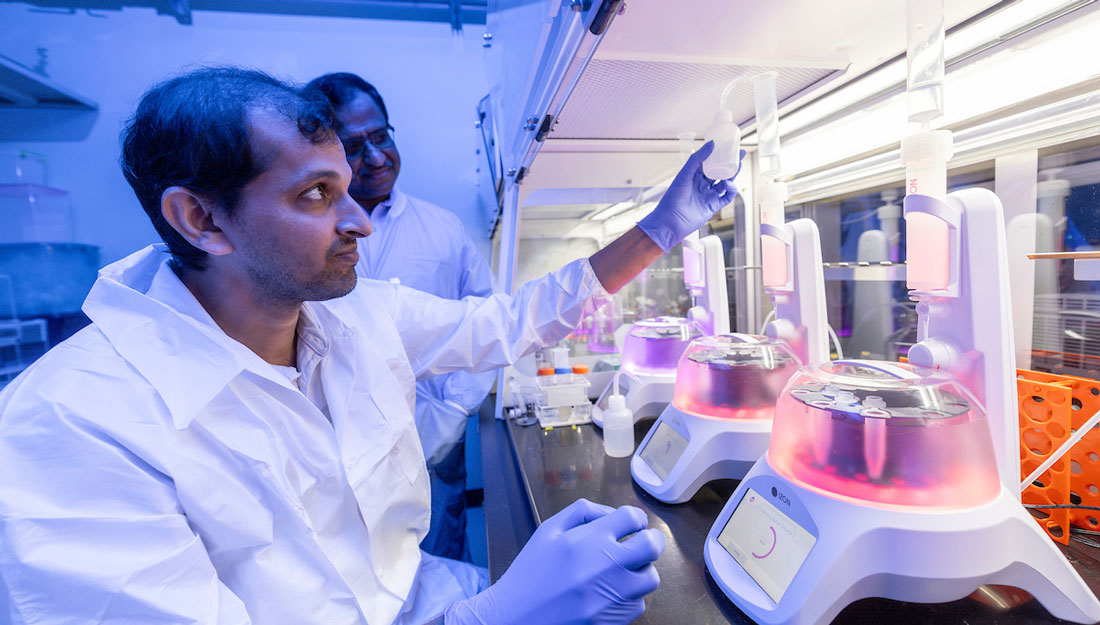
Lead researcher Ashok Shetty has filed a patent on the intranasal application of neural stem cell-derived extracellular vesicles for treating Alzheimer’s and other neurological and neurodegenerative disorders. (Abbey Santoro/Texas A&M University Division of Marketing & Communications)
Alzheimer’s disease is a leading cause of death among those aged 65 or older. As the most common form of dementia, Alzheimer’s accounts for an estimated 60 to 80 percent of cases and afflicts nearly 7 million Americans. The disease is characterized by progressive cognitive deficits, including issues with memory, communication and judgment, along with changes in mood, personality and overall behavior.
Despite its widespread prevalence, Alzheimer’s still lacks treatment options that effectively slow or stop its progression. To combat this, researchers at the Texas A&M University College of Medicine are exploring a new therapy to delay progression, publishing their findings in the Journal of Extracellular Vesicles.
Alzheimer’s results from progressive loss of neurons in the brain, an issue thought to be linked to abnormal accumulation of pathological proteins such as amyloid-beta and phosphorylated form of Tau and an incessant chronic inflammation in the brain. Amyloid-beta is a fragment of a larger protein called the amyloid precursor, which is important for brain development. In the brain of someone with Alzheimer’s, clumps of these amyloid precursor fragments accumulate between the neurons—referred to as amyloid-beta plaques—and disrupt their function. Similarly, the protein Tau is naturally expressed in healthy brains and helps stabilize and transport molecules through neurons. In the Alzheimer’s brain, however, Tau proteins stick together, creating neurofibrillary tangles and blocking the neuron’s transport system. Alzheimer’s patients also experience stronger inflammatory responses in the brain, which accelerates the loss of synapses—the connections that allow neurons to communicate—and leads to more neuron damage.
Madhu LN, PhD, is a research scientist and collaborator in the laboratory of Ashok K. Shetty, PhD, a University Distinguished Professor and associate director at the Institute for Regenerative Medicine in the Department of Cell Biology and Genetics. Together, Madhu, Shetty and their team of researchers aimed to target the chronic neuroinflammation seen in Alzheimer’s and find a method to improve brain function. Their approach utilized anti-inflammatory extracellular vesicles from human induced pluripotent stem cell-derived neural stem cells to non-invasively target cells perpetuating chronic neuroinflammation.
Neural stem cells can develop into either neurons or support cells in the brain, at which point, they release nanosized particles containing different active components. Previous research in Shetty’s lab found that extracellular vesicles contain microRNAs and proteins, which play a role in reducing neuroinflammation. They do this either directly by interacting with inflammatory pathways or indirectly by regulating cellular processes that help control inflammation in the brain or nervous system. Such cargo makes neural stem cell-derived extracellular vesicles a potential therapeutic for neurodegenerative diseases.
“The key point is that the secreted factors from human neural stem cells, enclosed in tiny extracellular vesicles released by these cells, could be utilized to treat Alzheimer’s disease through a non-invasive intranasal delivery method,” Shetty said. “This approach is effective because the cargo carried by these extracellular vesicles could reduce the neuropathological changes in the brain.”
These extracellular vesicles could be delivered through a simple nasal spray, Shetty said.

To test the results of this potential treatment, Madhu and colleagues administered these extracellular vesicles to an animal model of Alzheimer’s in the early stage of the disease. After administration, the team found decreased inflammation in the brain, fewer amyloid-beta plaques and lower levels of accumulated Tau. They also noted improved cognition, memory and mood.
The study also demonstrated that microglia, resident immune cells in the brain, incorporated intranasally administered neural stem cell-derived extracellular vesicles. Microglia play a major role in maintaining brain health by refining synapses, which are specialized junctions between neurons that promote neural network activity. They also protect against harmful microorganisms and clear cellular debris and misfolded proteins, including amyloid plaques.
In Alzheimer’s disease, when microglia encounter amyloid plaques, they become activated and release multiple proteins that cause inflammation. Initially, this activation helps clear amyloid plaques more quickly.
“However, prolonged activation causes them to lose their normal function and begin to harm neurons, leading to progressive neuron loss,” Shetty said.
Findings indicate that an intake of neural stem cell-derived extracellular vesicles significantly changed microglia gene expression related to Alzheimer’s and reduced the multiple harmful proinflammatory proteins without affecting their ability to clear amyloid-beta protein, Madhu said.
“Such alteration in microglia also prevented the overactivation of astrocytes, another type of brain cell that typically supports neurons but can become harmful in Alzheimer’s disease,” Madhu said.
Shetty has filed a patent on the intranasal application of neural stem cell-derived extracellular vesicles for treating Alzheimer’s and other neurological and neurodegenerative disorders. Their findings are already inspiring further studies, with ongoing research on Alzheimer’s disease in Shetty’s laboratory at the Texas A&M College of Medicine funded by the National Institute on Aging.
Next steps will include administering intermittent treatment to animal models at different stages of Alzheimer’s progression to determine if the treatment might lead to better cognitive function for prolonged periods, Shetty said. Successful findings in these upcoming studies could point toward treatment delaying Alzheimer’s-related changes and severe cognitive issues in humans by 10 to 15 years after the initial diagnosis.
“Our journey to advance the application of this therapy for Alzheimer’s disease is just beginning,” Shetty said.
Media contact: media@tamu.edu


